Abstract
Introduction
Allogeneic hematopoietic cell transplantation (HCT) is the only potentially curative treatment for many high-risk hematologic malignancies. Myeloablative conditioning is currently the standard of care for young and fit patients; however, graft-versus-host disease (GVHD) continues to be a major limitation to the success of HCT, increasing post-transplant morbidity and mortality. An ideal HCT is one combining strategies that reduce incidence and severity of GVHD, without compromising graft-versus-tumor effect.
We hypothesized that GVHD prophylaxis regimen consisting of post-transplant cyclophosphamide (PTCy), tacrolimus (Tac) and mycophenolate mofetil (MMF) will reduce the incidence of chronic GVHD in patients receiving a standard hematopoietic myeloablative HCT without an increase in risk of malignant relapse.
Methods
This is an interim analysis of a phase II study using a myeloablative preparative regimen of either: 1. total body irradiation (TBI, total dose 1320 cGy administered twice a day from days -4 to -1) or 2. Busulfan 3.2mg/kg daily (cumulative AUC 19,000 - 21,000 µmol/min/L) plus fludarabine 160mg/m 2 days -5 to -2 for patients unable to receive further radiation, followed by a GVHD prophylaxis regimen of PTCy (50mg/kg days +3 and +4), Tac and MMF (beginning day +5). The primary endpoint is cumulative incidence of chronic GVHD requiring systemic immunosuppressive treatment at 1 year post-transplant.
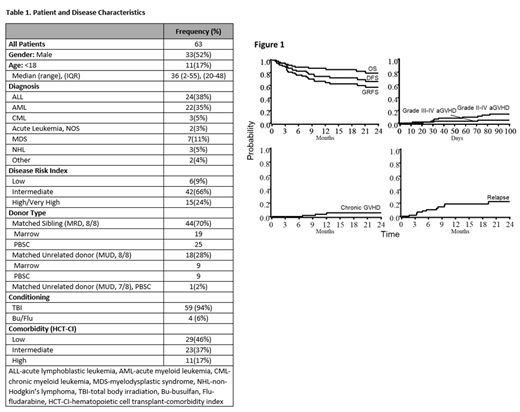
Patient and disease characteristics are detailed in Table 1. Eligibility included: age ≤ 60 years, malignant or non-malignant diagnosis, matched related (MRD) or unrelated (MUD) donor with either a bone marrow (BM) or filgrastim-mobilized peripheral blood (PB) graft.
Results
Through October 2020 we treated 63 patients with a median follow up of 502 days post-transplant. Of those, 48% were female and n=11 (17%) younger than 18 with median age at HCT of 36 years (range, 2-55; Interquartile range [IQR], 20-48). Donor source was 8/8 MRD in 44 patients (70%), 8/8 MUD in 18 (29%), and one with 7/8 MUD. Graft source was BM in n=28 (44%) and PB in n=35 (56%). Preparative regimen was TBI in 94% of patients.
All patients achieved primary neutrophil engraftment by 42 days, median 16 days (range, 13-27). Overall, 94% achieved platelet engraftment by 6 months, median 25 days (range, 16-98). At day 100, 48 patients (86%) achieved full donor bone marrow chimerism (>95% donor DNA); 29 (52%) and 52 (95%) achieved full donor peripheral blood CD3 and CD33 chimerism (defined as >95% donor). 42 patients (66%) required total parenteral nutrition (TPN) for oral mucositis and regimen-related toxicities during their initial transplant admission.
Cumulative incidence of Grade II-IV acute GVHD by 100 days post-transplant was 14% overall (95% confidence interval CI: 6-23%), 7% for MRD and 32% for the MUD group; Grade III-IV acute GVHD was 5% overall (CI: 0-10%), similar for both MRD and MUD group. At 1 year, only two patients receiving a PBSC graft developed chronic GVHD requiring immune suppression, for a cumulative incidence of 3% overall, one in the MRD group and one in the MUD group. Two-year cumulative incidence of relapse was estimated at 21% overall, 22% and 16% for the MRD and MUD groups, respectively. Two year cumulative incidence of non-relapse mortality was 13% overall, 15% and 5% for MRD and MUD, respectively. Estimated 2-year overall survival was 79% overall (CI: 65-88%), 75% for the MRD group and 95% for MUD. Estimated 2-year GVHD-free relapse free survival (GRFS) was 57% overall (CI: 42-69%), 56% and 63% in the MRD and MUD groups, respectively.
Discussion
Myeloablative transplantation with a TBI preparative regimen, followed by a GVHD prophylaxis regimen of PTCy, Tac, and MMF results in very low incidence of chronic GVHD. Importantly, this regimen is feasible and effective for pediatric and adult patients. Further improvement in outcomes can be achieved by incorporating post-transplant relapse mitigating strategies as well as supportive care measures to decrease regimen-related toxicities.
Arora: Kadmom: Research Funding; Pharmacyclics: Research Funding; Syndax: Research Funding. Janakiram: Bristol Meyer Squibb, Kyowa Kirin, ADCT Therapeutics: Honoraria; FATE, Nektar Therapeutics: Research Funding. Smith: Astellas Gene Therapies: Current Employment. Bachanova: Incyte: Research Funding; KaryoPharma: Membership on an entity's Board of Directors or advisory committees; FATE: Membership on an entity's Board of Directors or advisory committees, Research Funding; Gamida Cell: Membership on an entity's Board of Directors or advisory committees, Research Funding. Brunstein: BlueRock: Research Funding; AlloVir: Consultancy; FATE: Research Funding; NANT: Research Funding; GamidaCell: Research Funding. MacMillan: Equilium: Other: DSMB member; Incyte: Consultancy; Jazz Pharmaceuticals: Consultancy. Miller: Sanofi: Membership on an entity's Board of Directors or advisory committees; Magenta: Membership on an entity's Board of Directors or advisory committees; ONK Therapeutics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Vycellix: Consultancy; GT Biopharma: Consultancy, Patents & Royalties, Research Funding; Fate Therapeutics, Inc: Consultancy, Patents & Royalties, Research Funding; Wugen: Membership on an entity's Board of Directors or advisory committees. Betts: Patent Disclosures: Patents & Royalties: B.C.B. holds a patent (WO2015120436A2) related to CD4+ T cell pSTAT3 as a marker and therapeutic target of acute GVHD. B.C.B. additionally holds a provisional patent (WO2017058950A1) related to the use of JAK inhibitors for rejection and GVHD prevention. . Vercellotti: Mitobridge, an Astellas Company: Consultancy, Research Funding; CSL Behring: Research Funding. Weisdorf: Fate Therapeutics: Research Funding; Incyte: Research Funding. Holtan: Generon: Consultancy; Incyte: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal